(協作聚測試沙盒)
| 工具箱 |
下列各项的文字格式及显示效果都在模板消息列表中,请点击展开
(以下带*号者,请加签名~~~~作结)
|
| |
协作目标:甲状腺素
- 原始:0字节
- 沙盒:25,381字节
来源搜索:“"甲狀腺素"”——Google:网页、新闻、学术、图书、图片;百度:网页、新闻、学术、图片;知网工具书;JSTOR;维基百科图书馆
| 聚会/Wiki协作聚/沙盒/甲状腺素 | |
|---|---|
| |

| |
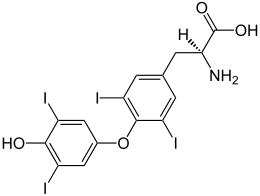
| IUPAC名 (2S)-2-amino-3-[4-(4-hydroxy-3,5-diiodophenoxy)-3,5-diiodophenyl]propanoic acid | |
| 识别 | |
| CAS号 | 7488-70-2 |
| PubChem | 853 |
| SMILES |
|
| MeSH | Thyroxine |
| 性质 | |
| 化学式 | C15H11I4NO4 |
| 摩尔质量 | 776.87 g·mol⁻¹ |
| 若非注明,所有数据均出自标准状态(25 ℃,100 kPa)下。 | |
甲状腺素是甲状腺激素之一,由酪胺酸和碘所组合而成的儿茶酚胺类激素,分为三碘甲状腺素(T3)及四碘甲状腺素(T4),T3的效果大概比T4强3到4倍。
碘为构成甲状腺素的主要成分,当缺乏时会造成甲状腺合成减少,引起甲状腺组织肿胀,即“缺碘性甲状腺肿”,俗称“大脖子病”。甲状腺素有促进细胞代谢,增加氧消耗,刺激组织生长、成熟和分化的功能,并且有助于肠道中葡萄糖的吸收。血液循环中的甲状腺素大多为半生期较长的T4。T3和T4在血液中的比例大约为1比20,而T4在细胞中会脱碘酶(deiodinase)转为活性较强的T3,并更进一步脱羧及脱碘形成3-碘类甲腺质(T1a)及类甲腺质 (T0a)。三种脱碘酶皆为含硒元素的酵素,因此硒元素的摄取在T3的制造上十分重要。
甲状腺功能亢进时,基础代谢增加造成内分泌旺盛,会有以下生理特征:头痛、神经紧张、心跳及呼吸加速、体重减轻、失眠、手抖、多汗、怕热、疲倦、凸眼、消化不良、腹泻等问题,需要减少对甲状腺素主要物质碘的摄取量。
甲状腺功能低下时,会有以下生理特征:体重上升怕冷、疲倦、嗜睡、体重增加、水肿、精神迟钝等症状。
东周时,中国已经有了关于甲状腺病的记载,在晋朝时,已经知道了用海藻可以治疗此病。
功能 编辑
甲状腺素几乎在身体上所有细胞作用,影响包括提高基础代谢率、影响蛋白质合成、协同生长激素造成骨骼的生长、促进神经的成熟以及提高身体对儿茶酚胺类激素(如肾上腺素)的敏感性。
甲状腺素在正常发育及细胞分化上扮演了重要的角色,它控制了蛋白质、脂肪以及碳水化合物的代谢,并且刺激维生素的代谢。数种生理上及病理上刺激影响了甲状腺素的合成。
制造 编辑
中枢 编辑
- 甲状腺球蛋白在粗糙内质网中合成,并经由胞吐作用进入到甲状腺滤泡腔的胶质中。
-同时,钠-碘泵经由主动运输将碘离子(I-)由血液唧入细胞
-碘离子利用碘离子通道经由促进性扩散进入滤泡腔[5]
-碘离子(I-)在胶质中被甲状腺过氧化酶(thyroid peroxidase)氧化为碘元素(I0)
-碘元素(I0)碘化了球蛋白的酪胺酰基(约120个).
-随后,毗邻的酪胺酰残基两两结合
- 复合体经由胞吐作用进入到了滤泡腔
- 蛋白酶将复合体进行切割,释出T4和T3
甲状腺素(T4 and T3)是甲状腺滤泡细胞(thyroid epithelial cell|follicular cell)所制造,受脑下腺前叶所释放的TSH调控。
T4(3,5,3',5'-tetraiodothyronine)是甲状腺滤泡细胞所制造,由甲状腺球蛋白所切割而得。
制造过程:
- 钠-碘泵唧出两个钠离子,同时唧入一个碘离子,并且碘离子以促进性扩散进入滤泡腔,为一次级主动运输。
- 甲状腺氧化酶(Thyroperoxidase)将碘离子( I-)氧化为碘元素( I2),以增加化学活性。
- 甲状腺氧化酶中碘化了甲状腺球蛋白的酪胺酰残基,并且在甲状腺滤泡细胞的内质网中两两结合,并且释出到胶质中。
- 脑下腺前叶释出促甲状腺素(TSH),结合于细胞膜的TSH受器上(一种G蛋白偶联受体),刺激甲状腺滤泡细胞对于甲状腺球蛋白的胞饮作用。
- 摄入的囊泡与甲状腺滤泡细胞的溶酶体结合,蛋白酶将碘化的球蛋白切割出T4。
- 最后,这些囊泡以胞吐作用释出甲状腺素。
甲状腺素是在酪胺酸的苯环接上碘而成,碘离子与钠离子经由反向运输进入滤泡细胞,使细胞内碘离子浓度达到血液中离子浓度的30倍。在甲状腺过氧化氢酶的作用下,形成单碘酪胺酸(monoiodotyrosine,MIT)以及双碘酪胺酸(diiodotyrosine,DIT),再结合形成甲状腺素。
流程:
- DIT + MIT → r-T3 (无生物活性)
- MIT + DIT → T3
- DIT + DIT → T4
周围 编辑
大多数的甲状腺素以T4型态存在于血液循环中,并在作用时转换为活性较强的T3,脱碘酶的缺乏将导致与碘摄取缺乏相同的症状。
胚胎的甲状腺素制造 编辑
Thyrotropin-releasing hormone (TRH) is released from hypothalamus by 6 - 8 weeks, and thyroid-stimulating hormone(TSH) secretion from fetal pitutary is evident by 12 weeks of gestation, and fetal production of thyroxine(T4) reaches a clinically significant level at 18–20 weeks.[6] Fetal triiodothyronine (T3) remains low (less than 15 ng/dL) until 30 weeks of gestation, and increases to 50 ng/dL at term.[6] Fetal self-sufficiency of thyroid hormones protects the fetus against e.g. brain development abnormalities caused by maternal hypothyroidism.[7]
碘缺乏对于甲状腺素合成的影响 编辑
If there is a deficiency of dietary iodine, the thyroid will not be able to make thyroid hormone. The lack of thyroid hormone will lead to decreased negative feedback on the pituitary, leading to increased production ofthyroid-stimulating hormone, which causes the thyroid to enlarge (the resulting medical condition is called endemic colloid goiter; see goiter). This has the effect of increasing the thyroid's ability to trap more iodide, compensating for the iodine deficiency and allowing it to produce adequate amounts of thyroid hormone.
循环及传讯 编辑
Plasma transport 编辑
Most of the thyroid hormone circulating in the blood is bound to transport proteins. Only a very small fraction of the circulating hormone is free (unbound) and biologically active, hence measuring concentrations of free thyroid hormones is of great diagnostic value.
When thyroid hormone is bound, it is not active, so the amount of free T3/T4 is what is important. For this reason, measuring total thyroxine in the blood can be misleading.
| Type | Percent |
|---|---|
| bound to thyroxine-binding globulin (TBG) | 70% |
| bound to transthyretin or "thyroxine-binding prealbumin" (TTR or TBPA) | 10-15% |
| albumin | 15-20% |
| unbound T4 (fT4) | 0.03% |
| unbound T3 (fT3) | 0.3% |
Despite being lipophilic, T3 and T4 cross the cell membrane via carrier-mediated transport, which is ATP-dependent.[8] The thyroid hormones function via a well-studied set of nuclear receptors in the nucleus of the cell, the thyroid hormone receptors.
T1a and T0a are positively charged and do not cross the membrane; they are believed to function via thetrace amine-associated receptor TAAR1 (TAR1, TA1), a G-protein-coupled receptor located in the cell membrane.
Another critical diagnostic tool is measurement of the amount of thyroid-stimulating hormone (TSH) that is present.
胞外传讯 编辑
Contrary to common belief, thyroid hormones can not traverse cell membranes in a passive manner like other lipophilicsubstances. The iodine in o-position makes the phenolic OH-group more acidic, resulting in a negative charge at physiological pH. However, at least 10 different active, energy-dependent and genetic-regulated iodothyronine transporters have been identified in humans. They guarantee that intracellular levels of thyroid hormones are higher than in blood plasma or interstitial fluids.[9]
胞内传讯 编辑
Little is known about intracellular kinetics of thyroid hormones. However, recently it could be demonstrated that thecrystallin CRYM binds 3,5,3′-triiodothyronine in vivo.[10]
Measurement 编辑
Thyroxine and triiodothyronine can be measured as free thyroxine and free triiodothyronine, which are indicators of thyroxine and triiodothyronine activities in the body. They can also be measured as total thyroxine and total triiodothyronine, which also depend on the thyroxine and triiodothyronine that is bound to thyroxine-binding globulin. A related parameter is the free thyroxine index, which is total thyroxine multiplied by thyroid hormone uptake, which, in turn, is a measure of the unbound thyroxine-binding globulins.[11]
甲状腺的影响 编辑
- Increases cardiac output
- Increases heart rate
- Increases ventilation rate
- Increases basal metabolic rate
- Potentiates the effects of catecholamines (i.e. increases sympathetic activity)
- Potentiates brain development
- Thickens endometrium in females
- increase metabolism of proteins and carbohydrates (i.e. they have a catabolic action[12])
医学用途 编辑
Both T3 and T4 are used to treat thyroid hormone deficiency (hypothyroidism). They are both absorbed well by the gut, so can be given orally. Levothyroxine is the pharmaceutical name (INN) of levothyroxine sodium (T4), which is metabolised more slowly than T3 and hence usually only needs once-daily administration. Natural desiccated thyroid hormones are derived from pig thyroid glands, and are a "natural" hypothyroid treatment containing 20% T3 and traces of T2, T1and calcitonin. Also available are synthetic combinations of T3/T4 in different ratios (such as liotrix) and pure-T3 medications (INN: liothyronine). Levothyroxine Sodium is usually the first course of treatment tried. Some patients feel they do better on desiccated thyroid hormones; however, this is based on anecdotal evidence and clinical trials have not shown any benefit over the biosynthetic forms.[13]
Thyronamines have no medical usages yet, though their use has been proposed for controlled induction of hypothermia, which causes the brain to enter a protective cycle, useful in preventing damage during ischemic shock.
Synthetic thyroxine was first successfully produced by Charles Robert Harington and George Barger in 1926.
处方 编辑
Today most patients are treated with levothyroxine, or a similar synthetic thyroid hormone.[14][15][16] However, natural thyroid hormone supplements from the dried thyroids of animals are still available.[16] Natural thyroid hormones have become less popular, due to evidence that varying hormone concentrations in the thyroids of animals before they are slaughtered leads to inconsistent potency and stability.[17][18] Levothyroxine contains T4 only and is therefore largely ineffective for patients unable to convert T4 to T3.[19] These patients may choose to take natural thyroid hormone as it contains a mixture of T4 and T3,[16][20][21][22][23] or alternatively supplement with a synthetic T3 treatment.[24] In these cases, synthetic liothyronine is preferred due to the potential differences between drug lots of natural thyroid products. It would be counterintuitive to supplement with T4-only if the patient cannot convert T4 to T3. Some natural thyroid hormone brands are F.D.A. approved, but some are not.[25][26][27] Thyroid hormones are generally well tolerated.[15] Thyroid hormones are usually not dangerous for pregnant women or nursing mothers, but should be given under a doctor's supervision. In fact, if a woman who is hypothyroid is left untreated, her baby is at a higher risk for birth defects. When pregnant, a woman with a low functioning thyroid will also need to increase her dosage of thyroid hormone.[15] One exception is that thyroid hormones may aggravate heart conditions, especially in older patients; therefore, doctors may start these patients on a lower dose & work up to avoid risk of heart attack.[16]
抗甲状腺素药物 编辑
Iodine uptake against a concentration gradient is mediated by a sodium-iodine symporter and is linked to a sodium-potassium ATPase. Perchlorate and thiocyanate are drugs that can compete with iodine at this point. Compounds such as goitrin can reduce thyroid hormone production by interfering with iodine oxidation.[28]
相关疾病 编辑
甲状腺素分泌过多或过少都会导致疾病:
- 甲状腺机能亢进(Hyperthyroidism):(如凸眼性甲状腺肿或称格雷夫斯症Graves Disease),甲状腺素释放过多所造成,大约2%的女性及0.2%的男性罹患此病。甲状腺毒症(Thyrotoxicosis)甲状腺毒症通常会被甲状腺机能亢进这个名词替换,但是彼此之间还是有些许的差异性存在,虽然甲状腺毒症也与甲状腺素分泌过多有关,主要原因是摄取过多甲状腺素的药片或者是甲状腺分泌过量,而甲状腺机能亢进则单指甲状腺分泌过量而已。
- 甲状腺机能低下有时会导致精神低落。[29] Some research[30] has shown that T3 is found in the junctions of synapses, and regulates the amounts and activity of serotonin, norepinephrine, and γ-aminobutyric acid (GABA) in the brain.
Preterm births can suffer neurodevelopmental disorders due to lack of maternal thyroid hormones, at a time when their own thyroid is unable to meet their postnatal needs.[31]
参见 编辑
T3和T4 编辑
外部链接 编辑
- Thyroxine bound to proteins in the PDB
甲状腺疾病的治疗
- Thyroid Hormone Treatment Brochure by the American Thyroid Association
- Elaborate article about the use of thyroid drugs Written by an MD
- What is the "Best" Thyroid Drug? Is it Synthroid, Unithroid, Armour, Thyrolar, or Something Else? Article by health activist and patient advocate Mary Shomon
- Thyroid Disease Manager Collection of elaborate medical articles on thyroid disease, including information on thyroid hormones
- Stop the thyroid madness Collection of references to articles comparing different treatment methods of hypothyroidism
参考文献 编辑
- ^ 参考
- ^ 空引用 (帮助)
- ^ References used in image are found in image article in Commons:Commons:File:Thyroid_systbcvhxcxcfffgem.png#References.
- ^ Chapter 48, "SYNTHESIS OF THYROID HORMONES" in: Walter F., PhD. Boron. Medical Physiology: A Cellular And Molecular Approach. Elsevier/Saunders. 2003: 1300. ISBN 1-4160-2328-3.
- ^ How Iodide Reaches its Site of Utilisation in the Thyroid Gland – Involvement of Solute Carrier 26A4 (Pendrin) and Solute Carrier 5A8 (Apical Iodide Transporter) - a report by Bernard A Rousset. Touch Brieflings 2007
- ^ 6.0 6.1 Page 493 (Table 33-3) in: Eugster, Erica A.; Pescovitz, Ora Hirsch. Pediatric endocrinology: mechanisms, manifestations and management. Hagerstwon, MD: Lippincott Williams & Wilkins. 2004. ISBN 0-7817-4059-2.
- ^ Zoeller RT. Transplacental thyroxine and fetal brain development. J. Clin. Invest. April 2003, 111 (7): 954–7. PMC 152596 . PMID 12671044. doi:10.1172/JCI18236.
- ^ "Plasma Membrane Transport of Thyroid Hormones and Its Role in Thyroid Hormone Metabolism and Bioavailability." Georg Hennemann, Roelof Docter, Edith C. H. Friesema, Marion de Jong, Eric P. Krenning and Theo J. Visser. Endocrine Reviews. August 2001; 22(4):451–476
- ^ Dietrich, J. W., K. Brisseau und B. O. Boehm (2008). "Resorption, Transport und Bioverfügbarkeit von Schilddrüsenhormonen" [Absorption, transport and bio-availability of iodothyronines]. Deutsche Medizinische Wochenschrift 133 (31/21): 1644-8.DOI 10.1055/s-0028-1082780
- ^ Satoru Suzuki, Nobuyoshi Suzuki, Jun-ichirou Mori, Aki Oshima, Shinichi Usami and Kiyoshi Hashizume. μ-Crystallin as an Intracellular 3,5,3′-Triiodothyronine Holder in Vivo. MMolecular Endocrinology April 1, 2007 vol. 21 no. 4 885-894. PMID 17264173
- ^ Military Obstetrics & Gynecology > Thyroid Function Tests In turn citing: Operational Medicine 2001, Health Care in Military Settings, NAVMED P-5139, May 1, 2001, Bureau of Medicine and Surgery, Department of the Navy, 2300 E Street NW, Washington, D.C., 20372-5300
- ^ http://www.ncbi.nlm.nih.gov/pubmed/2884552
- ^ "Thyroxine-triiodothyronine combination therapy versus thyroxine monotherapy for clinical hypothyroidism: meta-analysis of randomized controlled trials." Grozinsky-Glasberg S; Fraser A; Nahshoni E; Weizman A; Leibovici L. J Clin Endocrinol Metab. 2006 Jul;91(7):2592-
- ^ Robert Lloyd Segal, MD Endocrinologist
- ^ 15.0 15.1 15.2 "preferred thyroid hormone --Levothyroxine Sodium (Synthroid, Levoxyl, Levothroid, Unithroid)", Retrieved on 2009-3-27
- ^ 16.0 16.1 16.2 16.3 "Hypothyroidism Causes, Symptoms, Diagnosis, Treatment Information Produced by Medical Doctors", Retrieved on 2009-3-27
- ^ Cooper, DS. Thyroid hormone treatment: new insights into an old therapy.. JAMA. 1989, 261 (18): 2694–2695. doi:10.1001/jama.1989.03420180118042.
- ^ Clyde, PW; Harari AE, Mohamed Shakir KM. Synthetic Thyroxine vs Desiccated Thyroid -Reply (citing Cooper, DS, above). JAMA. 2004, 291 (12): 1445. doi:10.1001/jama.291.12.1445-b.
- ^ Thyroid hormone replacement therapy
- ^ "Consequences of Not Taking Thyroid Medications -Implications of Failing to Take Prescription Thyroid Drugs", Retrieved on 2009-3-27
- ^ "Armour Thyroid", Retrieved on 4-1-2009
- ^ "Nature-Throid", Retrieved on 4-1-2009
- ^ "Armour Thyroid Shortages Worsening: What Can Thyroid Patients Do?", Retrieved on 2009-3-27
- ^ Liothyronine
- ^ "Thyroid Information", Retrieved on 2009-3-27
- ^ "Desiccated thyroid in a nutritional supplement | Journal of Family Practice | Find Articles at BNET", Retrieved on 2009-3-27
- ^ "Nature-Throid", Retrieved on 4-1-2009
- ^ Spiegel C, Bestetti GE, Rossi GL, Blum JW. Normal circulating triiodothyronine concentrations are maintained despite severe hypothyroidism in growing pigs fed rapeseed presscake meal. J. Nutr. September 1993, 123 (9): 1554–61. PMID 8360780.
- ^ Kirkegaard C, Faber J. The role of thyroid hormones in depression. Eur J Endocrinol. 1998, 138 (1): 1–9. PMID 9461307. doi:10.1530/eje.0.1380001.
- ^ Dratman M, Gordon J. Thyroid hormones as neurotransmitters. Thyroid. 1996, 6 (6): 639–47. PMID 9001201. doi:10.1089/thy.1996.6.639.
- ^ Berbel P, Navarro D, Ausó E, Varea E, Rodríguez AE, Ballesta JJ, Salinas M, Flores E, Faura CC, de Escobar GM. (2010).Role of late maternal thyroid hormones in cerebral cortex development: an experimental model for human prematurity. Cereb Cortex. 20(6):1462-75. PMID 19812240.
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||



